Trigeminal Neuralgia: Treatment Options
Houston, Texas (TX), USA
Trigeminal neuralgia is a very debilitating disease. It is the most
common facial neuralgia in patients over 50 years of age. It occurs in
4 in 100,000 people, and is diagnosed mainly by history. It is often
caused by compression of the entry zone of a nerve supplying sensation to
the face (trigeminal nerve) by a blood vessel. In most cases, the
blood vessel responsible is the superior cerebellar artery, but in a small
portion of cases, the offending vessel may be a vein.

The picture above depicts the intense pain of trigeminal neuralgia, which
can be caused by even the slightest trigger, such as putting on makeup,
eating, chewing, drinking, kissing, etc. The shocks of pain
experienced in trigeminal neuralgia can last a few seconds, or minutes, or
longer. The pains do subside, and the patient does experience pain
free intervals. Trigeminal neuralgia is best diagnosed by history.
Lab tests do not diagnose this condition. Rather, trigeminal neuralgia
is diagnosed by the history and exam of an experienced physician.
\
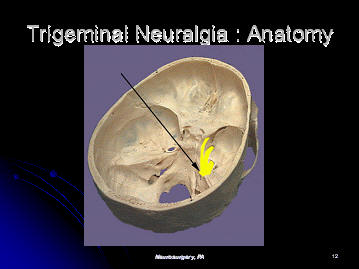
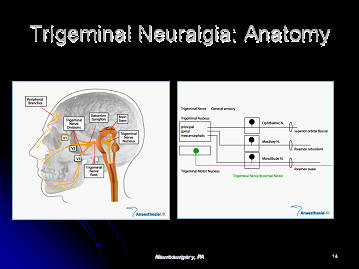
The trigeminal nerve leaves the brainstem, and exits the base of the
skull to supply sensation to the face. It divides into three divisions
of the trigeminal nerve, known as the ophthalmic, maxillary and mandibular
divisions of the trigeminal nerve. The ophthalmic portion of the
trigeminal nerve supplies sensation to the forehead and cornea of the eye.
The maxillary portion of the trigeminal nerve supplies the cheek. The
mandibular division of the trigeminal nerve supplies the jaw.
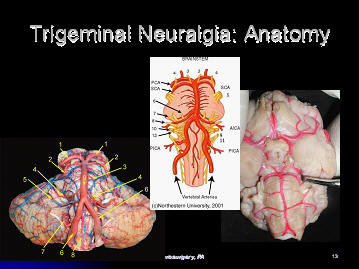
Above, the trigeminal nerve is seen leaving the brainstem.
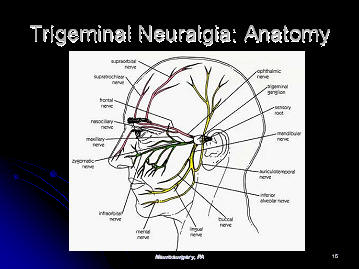
The anatomy of the trigeminal nerve is seen. The pink nerve is the
ophthalmic portion of the trigeminal nerve, the green is the maxillary
portion, and the yellow is the mandibular portion of the trigeminal nerve.
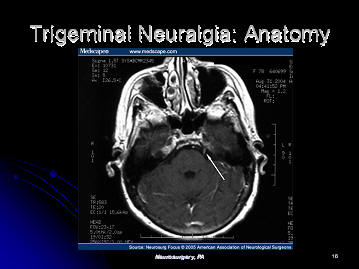
On the cross sectional MRI scan through the brainstem, one can see the
trigeminal nerve (shown with an arrow). The trigeminal nerve is small,
but the gamma knife is accurate enough to be
able to hit the nerve.
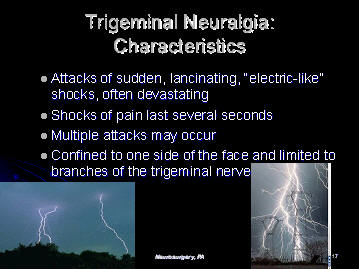
Typically, the attacks of trigeminal neuralgia consist of sudden,
lancinating, electric like shocks, which last several seconds.
Multiple attacks may occur, but the pain is confined to one side of the
face. The patient does not experience numbness over the face.
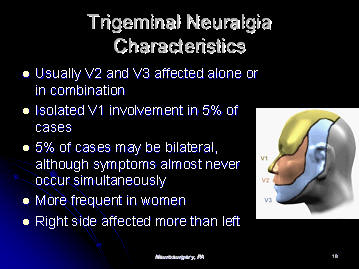
As is seen, there are three regions of the face, each supplied by a
different branch of the trigeminal nerve. Usually, V2 and V3 are
affected alone or in combination. Isolated involvement of V1 occurs in
5% of cases. Trigeminal neuralgia is more frequent in women than in
men. The right side is affected more than the left.
Trigeminal neuralgia is precipitated or triggered by several factors.
These include movement or stimulus to the eyebrow, upper lip, washing
the face, shaving, brushing the teeth, talking or eating. Even a
slight draft of wind may precipitate the trigeminal neuralgia.
Trigeminal neuralgia attacks often occur after the patient arises in the
morning. It does not wake patients from their sleep, however.
Trigeminal neuralgia typically occurs in patients over 50. In
younger patients with these symptoms, one must rule out multiple sclerosis
or a cerebellopontine angla (CPA) tumor.
In a patient experiencing trigeminal neuralgia, the neurological exam is
typically normal. Again, the diagnosis of trigeminal neuralgia rests
mainly in the history of the patient, and is recognized by the physician.
CT scans and MRI scans of the brain may be obtained to rule out another
type of pathology. Often, an MRI scan of the brain, with contrast,
will show a blood vessel loop compressing the root entry zone (where the
nerve enters the brainstem) of the trigeminal nerve.
Medical treatment is the usual initial treatment of trigeminal neuralgia.
One treatment of trigeminal neuralgia involves placing a needle into the
gasserian ganglion (from where the trigeminal nerve leaves), and causing
damage to the gasserian ganglion with either a chemical (glycerol) or with
heat (radiofrequency lesion). This often causes numbness in the region
which previously had pain.
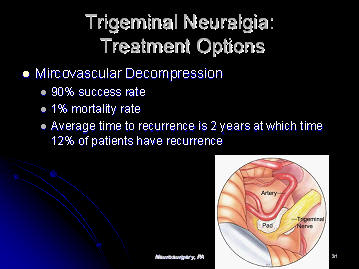
Another treatment for trigeminal neuralgia is a microvascular
decompression of the trigeminal nerve, otherwise known as the Janetta
procdure, named after its inventor. This procedure involves opening up
the back of the brain, moving the cerebellum over slightly, and dissecting
out the trigeminal nerve. One usually then finds a blood vessel
(usually the superior cerebellar artery) compressing the nerve where it
enters the brainstem. The neurosurgeon then dissects the blood vessel
off of the nerve, and places a small piece of Teflon mesh between the nerve
and the blood vessel. This procedure has a roughly 90% chance of
success, with a mortality rate of roughly 0.7%.
Gamma Knife is an excellent treatment option for trigeminal neuralgia.
The success rate is roughly 80%-85%, and the risk is minimal. The
improvement in pain is not immediate, but can take from several days, up to
three months after treatment.
This is a half day treatment. The patient enters the Gamma Knife
department, and a frame is placed on the head. A detailed MRI scan of
the brain is done, focusing upon the trigeminal nerve. A treatment
plan is then formulated by the neurosurgeon, radiation oncologist and
physicist. The treatment is then delivered, and the patient is
discharged home.
Treatment options for trigeminal neuralgia range from medication to
rhizotomy, to open microvascular decompression of the trigeminal nerve
leaving the brainstem, to Gamma Knife radiosurgery.
Gamma Knife has an 80% to 85% chance of having a good to excellent
result. The likelihood of complications using the Gamma Knife is low.
With Gamma Knife, the patient undergoes the procedure, and returns home
the same day. The effects of treatment can take from days, up to 3
months to occur.
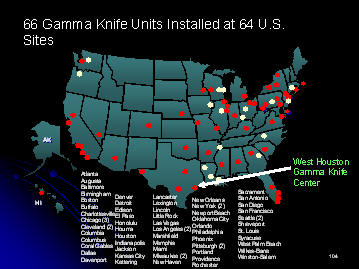
At the West Houston Medical Center Gamma Knife facility, we are
experienced at performing Gamma Knife Radiosurgery Procedures for trigeminal
neuralgia.
Gary Kraus, M.D. is the medical director of the Gamma Knife Center at
West Houston Medical Center. Dr. Kraus' experience with Gamma Knife
started in 1999, when he started and directed the Gamma Knife Center at the
Wallace Kettering Neuroscience Institute, in Dayton, Ohio. Under his
direction, the center performed over 500 Gamma Knife procedures. At
West Houston Medical Center, Dr. Gary Kraus is the medical director of the
Gamma Knife Center, and the medical director of Neurosciences. He has
10 years of experience in treating trigeminal neuralgia with Gamma Knife.
Treatment of trigeminal neuralgia with Gamma Knife is
an area in which Gary Kraus M.D. has extensive experience. He sees
patients at three offices in Houston Texas which are conveniently
located on the medical campuses of West Houston Medical Center, and Memorial
Hermann Memorial City Hospital, as well as in Katy, Texas. His
office serves patients in the Houston area, surrounding areas in
Texas, as well as other states in the United States, and abroad.
Please contact us at 281-870-9292, to help with your travel and hotel
arrangements.
|

