Gamma Knife
Houston, Texas (TX), USA
Gamma Knife stereotactic
radiosurgery is an alternative to
open brain surgery, in many cases. It is very useful at treating
certain benign and malignant tumors of the brain (acoustic neuromas,
meningiomas, metastatic brain tumors), facial pain (trigeminal neuralgia),
blood vessel malformations of the brain (AVM, or arteriovenous
malformations). The Gamma Knife consists of 201 beams of radiation,
emitted by radioactive cobalt, focusing on one area of the brain.
Generally, patients go home the same day. The name Gamma Knife
radiosurgery is derived as follows. The gamma rays are the energy
beams which focus upon the lesion, and are derived from radioactive cobalt.
The term radiosurgery comes from the fact that the reaction of the targeted
tissue is more similar to the reaction the tissue would undergo from a
surgery (where brain tumor is removed) than from traditional radiation
therapy. Stereotactic means that the beams of radiation all focus upon
one point.
My experience with Gamma Knife radiosurgery began in
June, 1999, when I started the Gamma Knife program at the Wallace Kettering
Neuroscience Institute, at Kettering Medical Center, in Kettering Ohio.
I trained at the Gamma Knife Center under Dr. Bengt Karlsson at the
Karolinska Insttitue in Stockholm, Sweden. I also trained at the Gamma
Knife Center at the Cleveland Clinic under Dr. Gene Barnett. While I was medical director of the Gamma Knife facility at Kettering
(Wallace Kettering Neuroscience Institute), the
center had performed over 500 Gamma Knife procedures. I have always
been very impressed with this incredibly accurate machine, which I feel
gives patients with certain lesions and disorders of the brain, a good
chance for success, with relatively low risk.
In November, 2004, I moved to Houston , Texas, to
develop and become Medical Director of the Neuroscience Center, and
Medical Director of the Gamma Knife Center, at West Houston
Medical Center. The Gamma Knife Center has the Model C Gamma Knife,
which one of the most sophisticated Gamma Knife units, allowing for the incredible
precision and accuracy of the Gamma Knife Models U and B (earlier models of
the Gamma Knife), with the addition of an Automated Positioning System,
which reduces the time the patient is in the Gamma Knife room during
treatment.
The number of patients treated worldwide, with the
Gamma Knife, is increasing on an exponential basis.
Here in Houston, we treat patients from the Houston
area, as well as from other states and abroad.
If you would like more information about Gamma Knife,
and whether it may be of benefit to you, please contact the office of
Gary E. Kraus, M.D.
neurosurgeon
Neurosurgery, P.A.
Medical Director, Neuroscience Center
Medical Director, Gamma Knife Center
West Houston Medical Center
Houston, Texas
Clinical Assistant Professor
Department of Neurosurgery
University of Texas Medical School at Houston
Houston, Texas, USA
tel: 281-870-9292
fax: 281-870-8493
website:
neurosurgerypa.com
The Gamma Knife Team in Houston Texas supports the treatment of
patients within the greater Houston area, Texas, many regions of the United
States, as well as Mexico and Puerto Rico. There is easy access for
international patients from Saudi Arabia and Dubai. If there are any questions,
please contact us. We would be happy to help with the arrangement of
hotel and transportation accomodations. For patients from Mexico or
Puerto Rico, we are very capable of handing any language barriers, to make
the treatment and stay as easy and pleasant as possible.
Below is a description of the benefits and merits of
the Gamma Knife. Many of the pictures were supplied by
Elekta, the company headquartered in Sweden, which manufactures the
Gamma Knife. Credit for the pictures goes to Elekta, and
these pictures are used with their permission.
Gamma Knife Radiosurgery
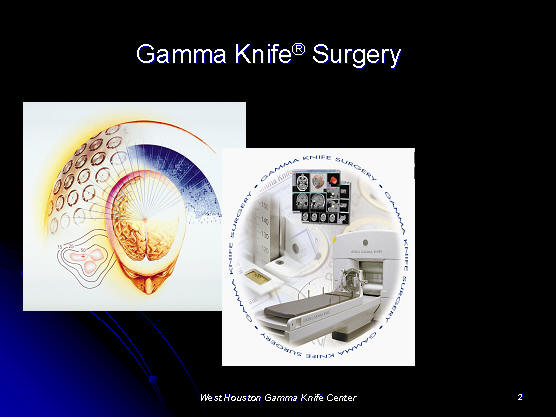
Dr. Gary Kraus practices Gamma Knife Surgery at the West
Houston Gamma Knife Center, in Houston, Texas. He is part of the Gamma
Knife Team.
The Gamma Knife is useful in the treatment of patients
with the following:
malignant
brain tumor (metastatic brain tumor, primary brain tumor)
benign brain
tumor ( acoustic neuroma, meningioma )
trigeminal
neuralgia (facial pain)
arteriovenous
malformation (AVM)
other lesions
of the brain.
Center of Arc Principle
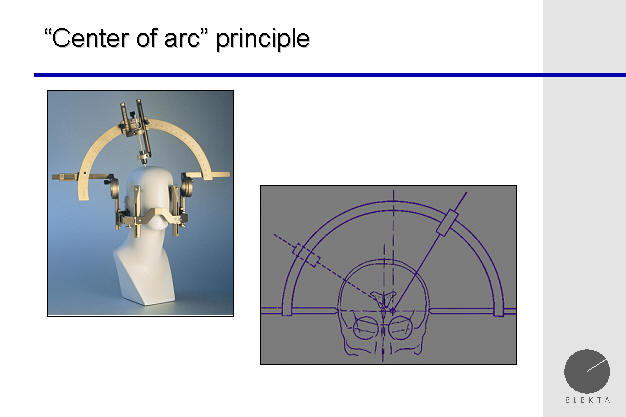
The Gamma Knife principles of operation are based upon
the "center of arc" principle, in which the center of the target is at the
center of the circular arc of rotation. This allows a "3 dimensional"
approach, otherwise known as a stereotactic approach to the brain. If
a biopsy needle is placed on the are, and passed into the brain, this is
then known as stereotactic neurosurgery. If, instead of a biopsy
needle, a beam of radiation is passed, this is then known as stereotactic
radiosurgery.
First stereotactic radiosurgery procedure
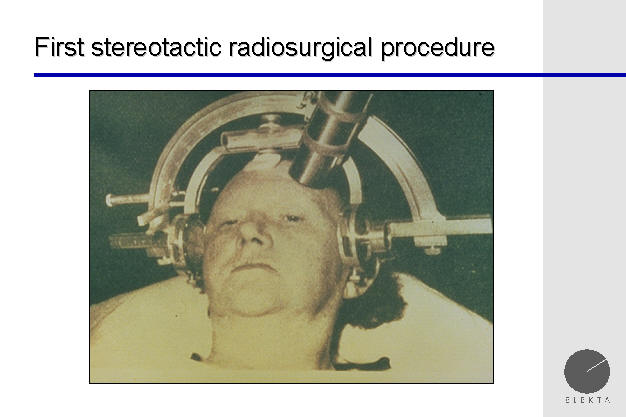
The performance of the first stereotactic radiosurgery procedure, before the invention of the Gamma Knife.
This was done by Dr. Lars Leksell, the neurosurgeon who invented the Gamma
Knife. The procedure was done at the University of Upsala, which had a
strong physics department, which was necessary to support the cyclotron used
in stereotactic radiosurgery.
Proton Beam Radiosurgery
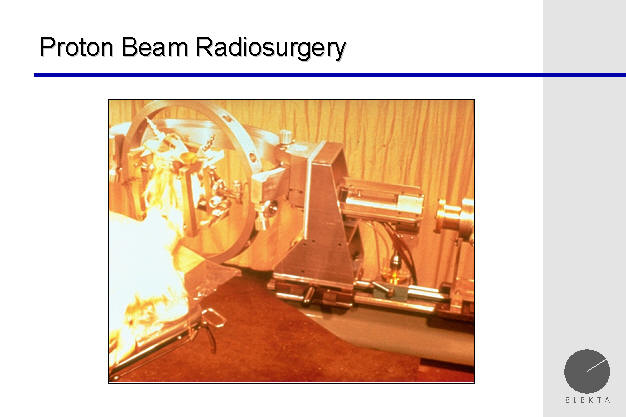
Dr. Lars Leksell had performed stereotactic proton
beam radiosurgery before developing the Gamma Knife. Proton beam
radiosurgery has significant uses today for certain tumors within the body.
Professor Lars Leksekk with the first Gamma Knife Unit, Stockholm, Sweden,
1968

Dr. Lars Leksell is seen with the first Gamma Knife
patient, in 1968, at the Karolinska Institute, Stockholm, Sweden.
Since Dr. Leksell didn't have the benefit of a cyclotron at the Karolinska
Institute in Stockholm, Sweden, he designed a device which became known as
the Gamma Knife, and which held fixed sources of gamma rays (cobalt) around
the patient's head.
First Installation of Gamma Knife Model U 1987 /
University of Pittsburgh
The first Gamma Knife was located at the University of
Pittsburgh, in 1987. This was the Model U. The use of the
Gamma Knife at the University of Pittsburgh was responsible for dramatically
increasing its use in the United States, and worldwide. Initial
research at the University of Pittsburgh lead the an exponential increase in
the acceptance of the Gamma Knife throughout the world.
Gamma Knife, Model B
The Model B Gamma Knife differs in design from the
Model U.
Gamma Knife, Model C
The Gamma Knife Model C has made the delivery of
stereotactic radiosurgery more efficient, by the addition of APS (automatic
positioning system). For most of the "shots" of radiation delivered,
the patient does not have the need for the Gamma Knife team to manually
change the position within the Gamma Knife Unit, but this is done instead,
automatically, by the machine itself.
Gamma Knife C, side view
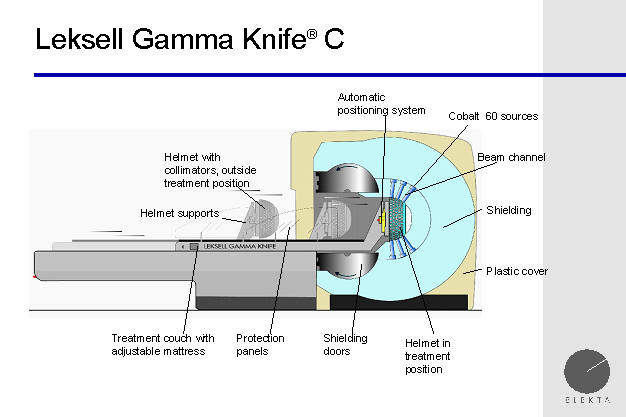
A cross section of the Gamma Knife shows the large
shielding ball, which contains the radioactive cobalt pellets, which provide
the radiation delivered by the Gamma Knife. The total weight of the
Gamma Knife ball is approximately 44,000 pounds.
Cobalt 60 radiation sources for Gamma Knife
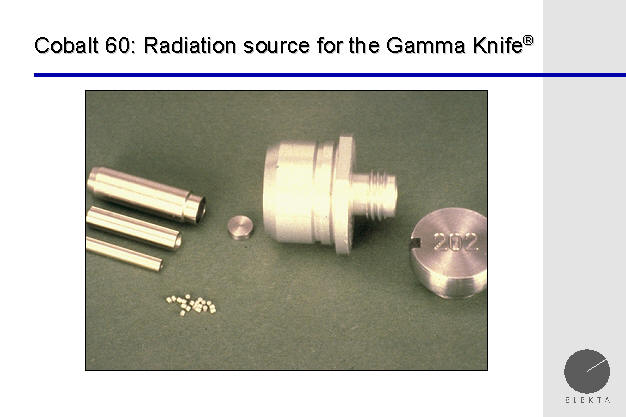
It is remarkable, that the total weight of the
radioactive pellets used within the Gamma Knife (for which 44,000 pounds of
steel are required for adequate shielding) is only 5 ounces. The half
life of the cobalt pellets is about 5.2 years, meaning that in this time,
they will lose half of their radioactivity.
Loading the Gamma Knife with cobalt pellets
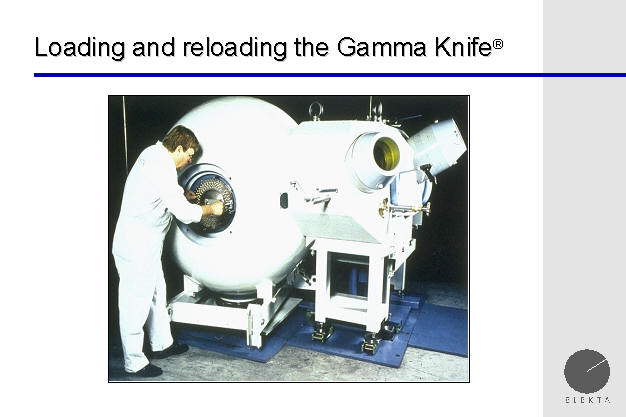
The loading process, during which the radioactive pellets
of cobalt are placed within the Gamma Knife Unit, is quite an involved
process, and may take several days. Here, the loading device is seen.
This device, seen next to the Gamma Knife, weights 16,000 pounds, and the
Gamma Knife itself weights 44,000 pounds.
Radiosurgery Principle
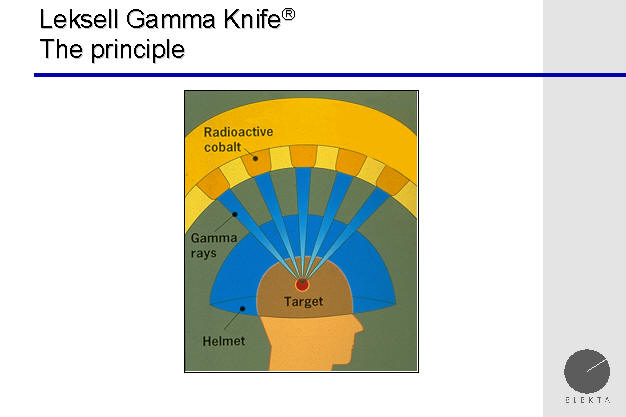
In the above schematic diagram, the beams of radiation
of the Gamma Knife are seen converging upon the target, which may be a brain
tumor, blood vessel disorder, or nerve. This is the principle of
stereotactic radiosurgery. This principle is also used by the
neurosurgeon when open neurosurgery is performed on the brain.
To better understand the principle of stereotactic
radiosurgery, consider the following example. Sunlight is not strong
enough to burn a hole in paper, but when we take a magnifying glass, and
focus the beams sunlight onto a single spot, now the focused energy can burn
a hole in paper. The same principle holds true for the Gamma Knife.
Each individual gamma ray of energy is, by itself, too weak to cause harm to
a brain tumor, or to the normal brain. But, when we focus 201 beams of
radiation energy together (on a brain tumor, or nerve (as in trigeminal
neuralgia), this area receives an enormous amount of radiation, with the
surrounding area of normal brain tissue receiving only a minimal dosage from
the several beams which pass through that area.
Steep Dose Profile
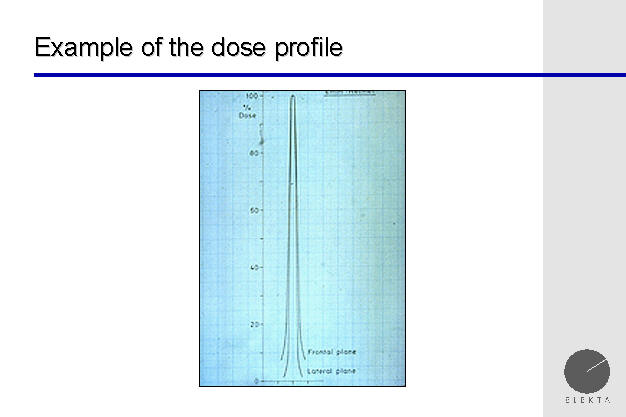
The accuracy of the Gamma Knife is demonstrated, by
showing the beam profile. Here we see, that even millimeters away from
the center of the target (which receives a great deal of radiation), the
brain tissue receives minimal amounts of radiation. This is very
important for protection of the normal brain tissue which may surround a
brain tumor.
Collimator Helmets for Gamma Knife

Above, the one of the helmets used in the Gamma Knife is
seen. This hold the collimators, which shape the beams of radiation.
The radiation passes through these ports, into the brain, and converge on
the brain tumor, blood vessel disorder, or trigeminal nerve (as in the
treatment of trigeminal neuralgia).
Collimators
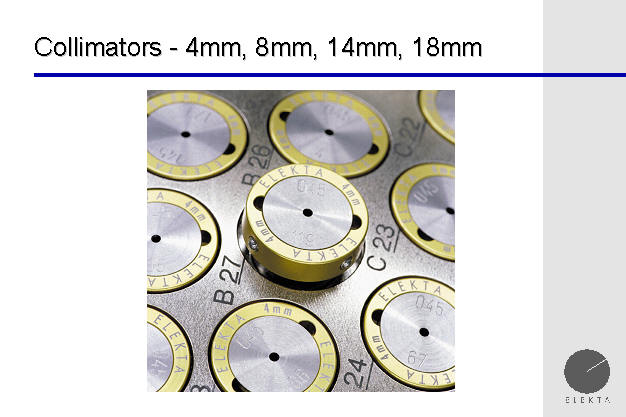
Above, the collimators are seem, which will shape the
beams, blocking all but a small portion of the individual beams of the Gamma
Knife, which allows for the accuracy of the Gamma Knife.
Lesion produced by gamma knife
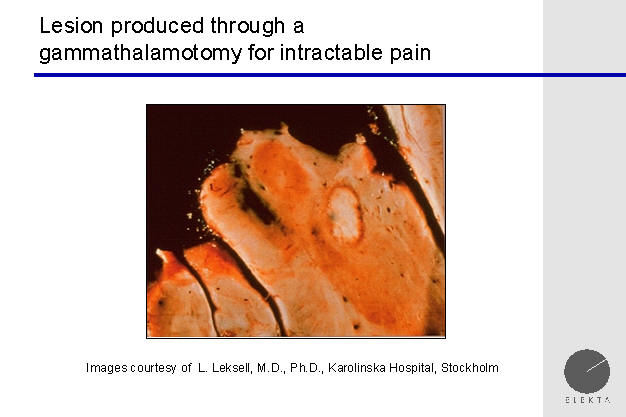
A cross section through a portion of the brain treated
with Gamma Knife, shows what appears to be a very focal lesion. This
is possible because of the accuracy of the Gamma Knife.
gamma knife radiosurgery / minimally invasive surgery on the brain

Above is a Gamma Knife collage, demonstrating the
focusing of beams, as well as a dose profile curve around a brain tumor.
teamwork for treatment
The Gamma Team consists of a team of whose team
members are an expert in their own field. The traditional Gamma Knife
Team will have an expert in Neurosurgery (neurosurgeon), Radiation Oncology, Physics, Neuroradiology and Nursing. The added expertise
of each individual helps to assure the patient of an accurate treatment,
benefiting from the input of an expert in each of the various specialties.
leksell stereotactic frame
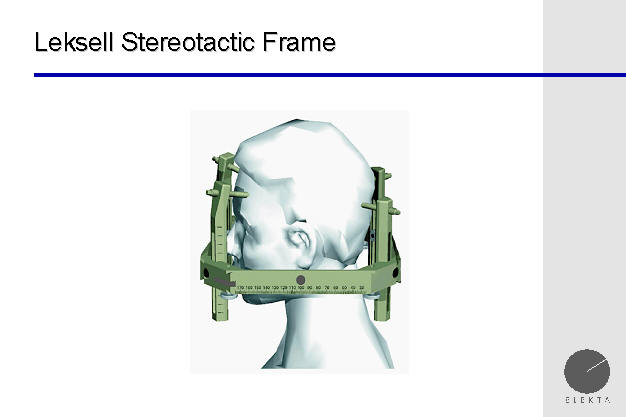
Here, the Leksell stereotactic frame is seen on a
patient's head. Placement of the frame takes several minutes, and,
depending upon the anesthetic used, many patients are not at all bothered by
it, and in fact, they often don't even remember it.
The rest of the day is "just boring" for the patient,
but it will not be painful.
diagnostic imaging: mri, ct, pet, angiography
The patient undergoes imaging studies. Above,
and MRI is being performed prior to the Gamma Knife procedure. The expert
team is looking for the brain tumor or blood vessel malformation, or
trigeminal nerve, upon which the radiation will be focused.
diagnostic testing
Imaging studies may consist of CT or MRI scans, and may
include angiography. In some cases, PET scanning may be added. A
brain tumor generally shows up better on an MRI scan that on a CT scan.
In particular, a metastatic tumor may show on an MRI scan, even when it is
extremely small in size. A CT scan is a good modality to see bone, and
may be used when a patient cannot undergo an MRI scan, such as is the case
if the patient has a pacemaker. An MRI is also valuable in visualizing
the trigeminal nerve, which is the target of the gamma knife for patients
suffering from trigeminal neuralgia.
finding the target / brain tumor
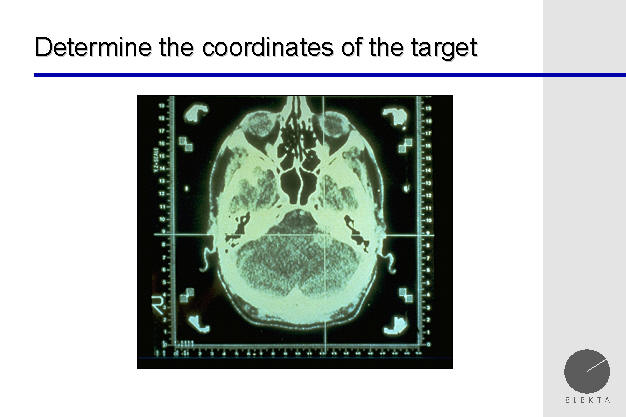
Above, a CT of the head is seen, with a Gamma Knife
Leksell frame already affixed to the patients head. The cross hairs
are focused on an acoustic neuroma, which is a benign brain tumor which
affects the hearing and balance nerve.
the gamma plan
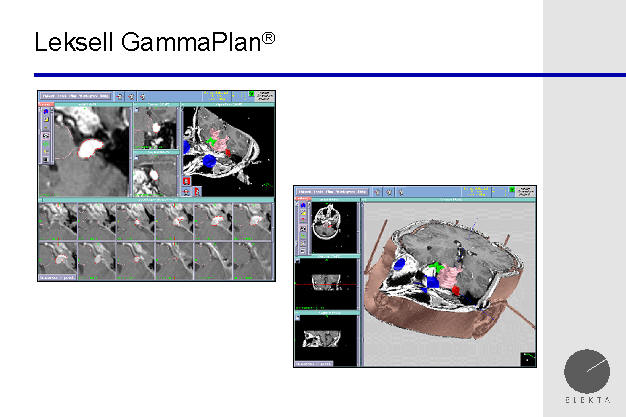
The Gamma Knife planning station software, which is
very sophisticated, allows modeling and simulation of the treatment outcome,
providing for the safety of treatment. This allows the delivery of
radiation to the target, but the minimization of radiation delivery to
critical structures, such as the optic nerves (nerves to the eyes).
Here, again, is seen a treatment plan targeting an acoustic neuroma.
An acoustic neuroma often presents when the patient notices a decrease in
hearing out of one ear. While hearing preservation is often difficult
with either open neurosurgery or gamma knife radiosurgery for an acoustic
neuroma, facial nerve function (which allows the face to move, smile, raise
the eyebrows, etc) is usually preserved with the Gamma Knife, while it is
often at risk with open neurosurgery.
patient ready for gamma knife treatment

Above, a patient is seen about to enter the Gamma
Knife. There is actually quite a bit of room, and the "closed in
feeling" which some patients experience with MRI scanners is not felt with
the Gamma Knife.
advantages of gamma knife radiosurgery
The Gamma Knife is becoming increasingly accepted as
the treatment for a number of disorders within the brain. There are
several reasons for this. The main reason is that it works, and it
provides for a good chance of success, with relatively low risk. The
other reasons include the cost advantage. There are no long
hospitalizations as is often the case with open brain surgery, and patients
often return home the same day. The risks of complications are
relatively low, especially compared with open brain surgery.
Essentially, Gamma Knife can be considered minimally
invasive brain surgery. Because it is minimally invasive, it is
sometimes referred to as "brain surgery without a scalpel."
indications for gamma knife
The Gamma Knife may make certain lesions, which
otherwise seem "inoperable" with conventional open surgery, now "operable"
with Gamma Knife Radiosurgery. Elderly patients, who want to avoid the
risks of a major open surgical procedure, may opt for Gamma Knife.
Gamma Knife may also be used to treat portions of
tumors or arteriovenous malformations (AVM's) which were not removed at the
time of an open surgical procedure.
The Gamma Knife is useful in the treatment of patients
with the following:
malignant
brain tumor (metastatic brain tumor, primary brain tumor)
benign brain
tumor ( acoustic neuroma, meningioma )
trigeminal
neuralgia (facial pain)
arteriovenous
malformation (AVM)
other
lesions.
Metastatic Brain Tumor : Houston, Texas
A metastatic brain tumor is a tumor which has spread
from another portion of the body. It may have come from the lung,
breast, colon, skin, or kidney, as well as other areas. When the
metastatic tumor spreads to the brain, it may grow there as a single lesion,
or may develop in different areas of the brain, as multiple tumors.
The greater the number of tumors, the more difficult it will be to treat.
On the other hand, the likelihood that a metastatic tumor will arrest its
growth, due to Gamma Knife radiosurgery, is roughly 90%. Even if the
tumors are on different portions of the brain, the brain tumors can be
addressed. There are many different protocols which are used to treat
metastatic tumors to the brain. Depending upon the nature of the
tumor, and its cells of origin, different treatments may be used.
Gamma Knife radiosurgery does play a mojor role in the treatment of brain
metastasis.
Trigeminal neuralgia is a debilitating condition, in
which a patient suffers lancinating, shock like pains, to a side of the
face. This affects only one side of the face, and may involve the
forehead, eye, cheek, maxillary or mandibular area. Often, chewing,
touching, brushing the teeth, and even the wind, may precipitate severe
spasms of facial pain, which will subsequently resolve. Patients with
trigeminal neuralgia typically have pain free intervals between the episodes
of extreme pain. Treatment options available for trigeminal neuralgia include:
1) medications such as tegretol or dilantin, 2) lesioning of the trigeminal
nerve with a needle, as in a trigeminal rhizotomy, 3) an open neurosurgery
procedure on the back of the brain, to move an offending artery away from
the base of the trigeminal nerve (this procedure is known as a microvascular
decompression (MVD) ), and 4) Gamma Knife radiosurgery. While an open
surgery as the highest chance for success (90%), it also has the highest
risk of complications. Gamma Knife radiosurgery has an 80% - 85% of
giving patients with trigeminal neuralgia a good to excellent result, with a good result being
reduced pain while still on medications, and an excellent result being no
pain off of medications.
With Gamma Knife radiosugery, the improvement in the
facial pain of trigeminal neuralgia is not immediate, but may take from days to weeks. If the
patient does not experience any pain relief after three months, the
procedure was not considered to be a success.
Acoustic Neuroma
An acoustic neuroma is a benign tumor which usually
grows from one of the nerve roots which travel to the vestibular apparatus
in the skull base, which is responsible for balance. The other nerves
which are in contact with this nerve are the facial nerve, which allows
movement of the face (as in smiling, frowning, etc), and the hearing nerve.
As the acoustic neuroma grows, hearing is often affected. There are
several different neurosurgery approaches which may be used in the treatment
of an acoustic neuroma, but, for appropriately sized tumors, the Gamma
Knife offers an excellent combination of a high chance of success, with a
low risk. The Gamma Knife has a 90% - 95% chance of arresting growth
of an acoustic neuroma. Occasionally, the tumor may appear on MRI
scans to be larger 6 months after gamma knife radiosurgery than it was
before gamma knife, but this is often swelling of the tumor from radiation
injury, and in most of these patients, as the tumor is followed one, two and
three years down the road, the tumor will begin to shrink.
gamma knife is often the treatment of choice
Gamma Knife is becoming the treatment of choice for
acoustic neuromas, which are slow growing benign tumors growing at the base
of the skull.
cost comparison gamma knife vs craniotomy
length of stay gamma knife vs craniotomy
Another nice advantage of the gamma knife for the
treatment of a brain tumor, or trigeminal neuralgia, is that the patient
will generally return home the same day. When the neurosurgeon
performs an open neurosurgery, the patient may be in the hospital for days.
For questions or additional information about Gamma
Knife, or if you would like to determine whether this treatment may be
appropriate for you or someone you know, please contact the office of
Gary E. Kraus, M.D.
neurosurgeon
Neurosurgery, P.A.
Medical Director, Neuroscience Center
Medical Director, Gamma Knife Center
West Houston Medical Center
Houston, Texas
Clinical Assistant Professor
Department of Neurosurgery
University of Texas Medical School at Houston
Houston, Texas, USA
Neurosurgeon:
West Houston Medical Center
Memorial Hermann Memorial City Medical Center
tel: 281-870-9292
fax: 281-870-8493
website:
neurosurgerypa.com
The Gamma Knife Team supports the treatment of patients
within the greater Houston area, Texas, many regions of the United States,
as well as Mexico and Puerto Rico. There is easy access for
international patients from Saudi Arabia and Dubai. If there are any questions, please
contact us. We would be happy to help with the arrangement of hotel
and transportation accomodations. For patients from Mexico or Puerto
Rico, we are very capable of handing any language barriers, to make the
treatment and stay as easy and pleasant as possible.
Dr. Kraus has 10 years of experience with Gamma Knife
Radiosurgery. He is medical director of the Gamma Knife Center at West
Houston Medical Center. There are three offices in Houston Texas which
are conveniently located on the medical campuses of West Houston Medical
Center, and Memorial Hermann Memorial City Hospital, as well as in Katy,
Texas. His offices serve patients in the Houston area,
surrounding areas in Texas, as well as other states in the United States,
and abroad. Please contact us at 281-870-9292, to help with your
travel and hotel arrangements.
|

