A patient's surgery experience
What to expect during surgery
 Surgery
involves a huge amount of trust in a complete stranger (the surgeon),
after meeting for only a brief period of time. If I were to say to you
"give me all your money, your car keys, and the deed to your house, and I'll
give them back to you tomorrow, you would say "what are you, nuts?"
And yet, each day, a patient will trust a surgeon, who has spoken with them
for literally minutes, to say that we will put them to sleep, make an
incision, get down to nerves, take out a disk or fuse the spine, close them
up, and then awaken them. Can there be a greater level of trust
bestowed upon one human by another? Surgery
involves a huge amount of trust in a complete stranger (the surgeon),
after meeting for only a brief period of time. If I were to say to you
"give me all your money, your car keys, and the deed to your house, and I'll
give them back to you tomorrow, you would say "what are you, nuts?"
And yet, each day, a patient will trust a surgeon, who has spoken with them
for literally minutes, to say that we will put them to sleep, make an
incision, get down to nerves, take out a disk or fuse the spine, close them
up, and then awaken them. Can there be a greater level of trust
bestowed upon one human by another?
Day of the operation:
Often, surgery will begin in the morning, unless the
operation is "following" another. A typical start time will be 7:30 AM
or 8:00 AM. The patient will have been instructed to not eat or drink
anything for at least six hours before surgery. This decreases the
risk of aspiration during the intubation process (the placement of a
breathing tube into the lungs, by the anesthesiologist).
The patient will often be given a sedative just before
going back to the operating room (OR). In the OR, there will be a lot
of activity, which might be disconcerting to the patient. What the
patient must remember is that all the activity in the room is for the
benefit of the patient. Everyone is focused on a particular task, in
order to make sure the patient has a safe and successful surgery. The
room may seem cool, and the personnel might appear impersonal, but this is
only because they are focused on a number of tasks.
Various lines may be placed. This means that the
patient might have additional intravenous (IV) lines started, to supply
fluid. A central line, which is essentially a large IV placed either
under the collar bone or into the jugular vein in the neck, might be
inserted. Although this sounds like a big deal, for an
anesthesiologist this is a routine task. A Foley catheter to drain the
bladder may be placed if the procedure is anticipated to last several hours.
An arterial line, which is essentially a line to measure arterial blood
pressure instantly, might be placed. Some of these lines might be
placed after the patient is put to sleep.
Next the patient will go to sleep. The
anesthesiologist will insert the endotracheal tube into the lungs (this will
breathe for the patient while asleep). The patient will then be
positioned appropriately for the surgery. For a posterior approach
surgery, the patient will be turned over into the prone position (on the
belly), with the knees, elbows, breasts and genitals carefully cushioned to
decrease the risk of pressure sores.
The surgeon will then usually mark the skin in the
region of intended incision. The circulating nurse will "prep" the
skin with antibiotic solution and scrub, and the scrub nurse will "drape"
the patient with towels and an iodine impregnated plastic "sticky" drape
known as ioban. The remainder of the body is now draped off.
While the body is being prepped and draped, the
surgeon will generally "scrub" his hands and forearms. He will then
enter the room, "don" his gown and gloves, step up to the field, and start
operating.

Seen here is a typical modern operating room.
The anesthesiologist is located behind the "ether screen." The blue
drape covers the patient. An IV pole is seen, from which fluids are
"hung."


The operating microscope has advanced the field of
microneurosurgery. It provides three advantages to the surgeon.
- magnification
- light
- stereoscopic vision
The ability to see in stereo is an important one.
The distance between one's pupils is roughly 55 mm, too large to see in
stereo in a small hole. The operating microscope evades this problem
for the surgeon.

Many instrument are used during a typical
neurosurgical operation. For this reason, it is one of the more
difficult specialties for scrub nurses to learn.

An extensive set of retractors is available to the
neurosurgeon. These help to keep the skin, fat and muscle retracted
while the surgeon is operating. As can be seen here, a variety of
depths of blades are required, depending on the size of the patient.

A Shaw Scalpel (top device) provides the ability to
cut with little blood loss. The blade heats up and coagulates fine
vessels when they are divided. The bipolar coagulator (bottom device)
allows the surgeon to coagulate between the tips of a fine instrument,
preventing electrical current from traveling to the rest of the body.

The Bovie coagulator (also known as monopolar) allows
coagulation, by sending electricity from the tip of the instrument to a
grounding pad (usually on the leg).

A cell saver allows a good portion of the blood which
is lost during the case, to be sucked up, processed, and given back to the
patient.

Nerve monitoring, usually left up to the discretion of
the surgeon, allows the evaluation of the integrity of the nerve roots,
while the patient is asleep.

Bone graft is seen here. This cancellous
material provides a good framework or lattice for the patients own bone to
grow through.

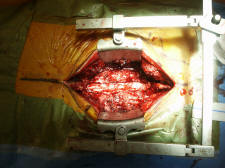
Although difficult to see, the lamina has been removed
during this posterior lumbar laminectomy, and the dura covering the spinal
nerves is visible.

Dr. Kraus is seen operating on a lumbar spine.
The operating microscope is seen on the right. An extremely
experienced team is assisting him.
Following closure of the wound, a dressing is applied,
and the patient taken to the recovery room. The surgeon will then
evaluate the patient, write orders, dictate the operative procedure, and
speak with the family.
|

